Thyroid and fertility (part 2)
Okay, so now that we know your thyroid is essential to your cycle, trying to conceive, and sustaining a healthy pregnancy, (if you missed part 1 of this thyroid series, click here to go read it!) let’s chat about what it looks like when your thyroid isn’t functioning at its best.
Symptoms that suggest your thyroid may need some support
The following symptoms can clue you in that your thyroid needs some lovin’. They include:
- unexplained weight loss
- unexplained weight gain
- irregular cycles
- infertility
- pregnancy loss
- heavy periods
- low BBT (below 97.5)
- brain fog
- hair loss
- dry skin
- brittle nails
- cold extremities
- lack of quality sleep
- sleep interruptions
- anxiety
If you’re reading this list and checked off three or more of these symptoms, it may be time to get your thyroid levels checked. The best way to do that is via bloodwork.
What labs to ask for to check thyroid levels?
The most popular test for checking thyroid is TSH or thyroid-stimulating hormone. That’s the hormone that helps your brain communicate with your thyroid (telling it to make more or less thyroid hormone). But that’s only one aspect of thyroid health. And the range conventional doctors use to determine “normal function” is wider than it should be – meaning your thyroid could be sluggish but deemed “normal”.
You want to ask for a full thyroid panel, which will include: TSH, total and free T4 (a major thyroid hormone), total and free T3 (the active form of thyroid hormone), thyroid antibodies (TPO and anti-Tg), and reverse T3 (the inactive form of thyroid hormone). This will give you a much more robust picture of how your thyroid is functioning.
What are some (maybe unintentional) things that could be sabotaging your thyroid?
- undereating
- overexercising
- skipping sleep
- skipping breakfast
- skipping carbs
What are some foundational ways to support your thyroid?
Some of the best ways to support your thyroid help to prevent unnecessary stress to the body and provide the thyroid with everything it needs (i.e. minerals!) to produce adequate thyroid hormone. They include:
- eat breakfast
- drink caffeine with breakfast
- adequate mineral intake
- don’t skip eating carbohydrates
What if you’ve had labs done and everything came back “normal” but you still have symptoms?
Conventionally speaking, thyroid levels may be deemed “normal” based on the current ranges provided. I like to see client’s thyroid functioning optimally, so the ranges I use are more conservative (i.e. smaller, more ideal numbers). So, you can have “normal” thyroid hormones on a conventional level but they may not on an optimal level.
Also, lab results are not end all be all. If you have normal labs but you’re still having symptoms, how you feel still matters (aka it’s not all in your head!) You can have normal thyroid function but since practically the entire body uses thyroid hormone, your cells may be struggling to effectively use that thyroid hormone. That comes down to your body’s stress response – emotionally, physically, mentally, illness, trauma, you name it, etc.
Okay, so that’s me. What should I do next?
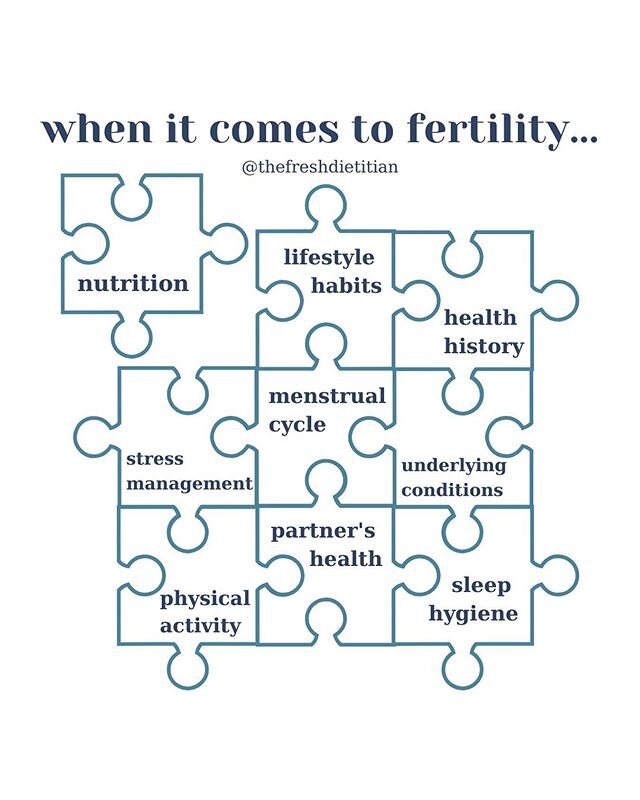
You’ll want to find the root cause of your stress (again could be coming from a number of different reasons) and then figuring out how to alleviate that stress. Figuring that out is so individual. I would recommend working with a practitioner who is familiar and comfortable with thyroid issues and who also focuses on a whole body approach. Diet and lifestyle are huge players here so it requires a deep dive into food habits and routines and stress analysis and ultimately stress management techniques.
Thyroid issues can be tricky. If you suspect your thyroid may be interrupting your ability to get pregnant or even preventing you from feeling your best after having babies, apply to work with me here.
Thyroid and Fertility 101 (part 1)
January is Thyroid Awareness Month.
But actually, it feels like that every month over here in my little corner of the internet because I so heavily emphasize getting it checked with nearly all of my clients.
It’s because the health of your thyroid plays a significant role in your ability to get pregnant and your ability to sustain a pregnancy.
Your thyroid is a butterfly-shaped gland located in front of your throat and releases thyroid hormones that serves various functions throughout the body.
Nearly every single cell uses thyroid hormone to help with metabolism (processing nutrients and energy). Your thyroid can also be described as the thermostat of the body due to its role in controlling your temp.
Your thyroid is involved in:
temperature regulation
heart rate
nutrient metabolism
brain function
menstrual cycles
growth and development (for you always and for your baby while pregnant)
…among many more roles!
I’ll be focusing on the roles your thyroid plays in menstrual cycles and pregnancy and what can happen when there are disruption in thyroid function.
But before we get into that, I’ll go over how the thyroid works (important to discuss how it works under normal circumstances so you better understand what’s going on when it’s not working properly).
How the thyroid works
Your brain and thyroid communicate via the HPT axis or hypothalamus-pituitary-thyroid axis). The hypothalamus released TRH (thyrotropin-releasing hormone) that stimulates the pituitary gland.
The pituitary gland then releases TSH (thyroid-stimulating hormone) that stimulates the thyroid to release T3 (20%) and T4 (80%) (and calcitonin but we’re skipping over that part). T3 is much more potent than T4 and is considered the active form of thyroid hormone.
T3 and T4 then travel throughout the body assisting cells in regulating their metabolism (among the many other roles listed above). Cells can also convert T4 to T3 or reverse T3 (the inactive form of thyroid hormone) depending on needs.
When concentrations of T3 and T4 in your bloodstream reach a certain level or threshold, they create a negative feedback loop to your brain. This shuts off the release of TRH, which then shuts down the release of TSH, decreasing the stimulation of your thyroid. Normal stimulation resumes again once T3 and T4 levels decrease.
This is a “picture perfect” version of how your thyroid (should) function. Of course, things don’t always work out that way!
Thyroid’s role in menstrual cycles
The thyroid’s role in menstrual cycles is complex…to say the least. I’ve tried to simplify it here but know this is surface level. It goes much deeper than this and there’s still so much we don’t know.
Thyroid hormone plays a role in how sex hormones are made, transported, and excreted. By sex hormones we’re talking major players like estradiol and testosterone.
Thyroid hormone also plays a role in controlling other hormones that indirectly influence your cycle. So, thyroid hormone can influence factors such as the length between periods (whether short or long or if your period shows up at all) to how light or heavy your period flow is.
Thyroid hormones also act directly on ovarian cells. One role is to help facilitate the recruitment and maturation of follicles (very important as those are the beginning stages of ovulation).
So, when there are disruptions in thyroid function, it can have several downstream impacts on your cycle, which can ultimately impair your fertility.
That’s where taking care of your thyroid is SO important when it comes to preconception health and at the core of what I look into with clients who are struggling to get pregnant.
Thyroid’s role in pregnancy
There is an increased demand for thyroid hormone during pregnancy.
In the early weeks of pregnancy (up to week 12), the fetus is dependent on your thyroid’s ability to provide it necessary hormones.
By week 12, the fetus is starting to make its own thyroid hormones but still not enough until about weeks 18-20 (meaning still heavily dependent on you).
Most importantly, the fetus needs thyroid hormone to have proper brain and nervous system development. (Remember above when I mentioned that every cell in the body uses thyroid hormone to function).
Your thyroid needs to be able to not only provide you enough hormone but the fetus, too (and have that amount of hormone be enough but not too much!
Bottom line: the function of your thyroid is crucial to sustaining a healthy pregnancy!
This month we’ll be getting into the ways to support your thyroid and what labs to ask for to assess function!
If you’re wanting support for your thyroid while TTC, apply to work with me here!
Your preconception checklist for getting pregnant in 2023
Track your cycle and know how to identify your fertile window
Knowing your cycle (period length, flow, consistency, color, cervical mucus, BBT, etc.) is vital to learning your fertile window so you’re able to time sex appropriately when you’re ready to start actively trying. Knowing your cycle can clue you into there being an issue if it’s irregular or changes occur outside of your norm. It’s arguably the most important step to take while TTC.
Take a high quality prenatal
Prenatal vitamins are an important piece of preconception nutrition in that they can fill some nutrient gaps and add to your nutrient stores prior to getting pregnant. Look for a prenatal that has adequate levels nutrients in forms that are absorbable. If you’d like help in choosing, download the list of my favorite prenatals here.
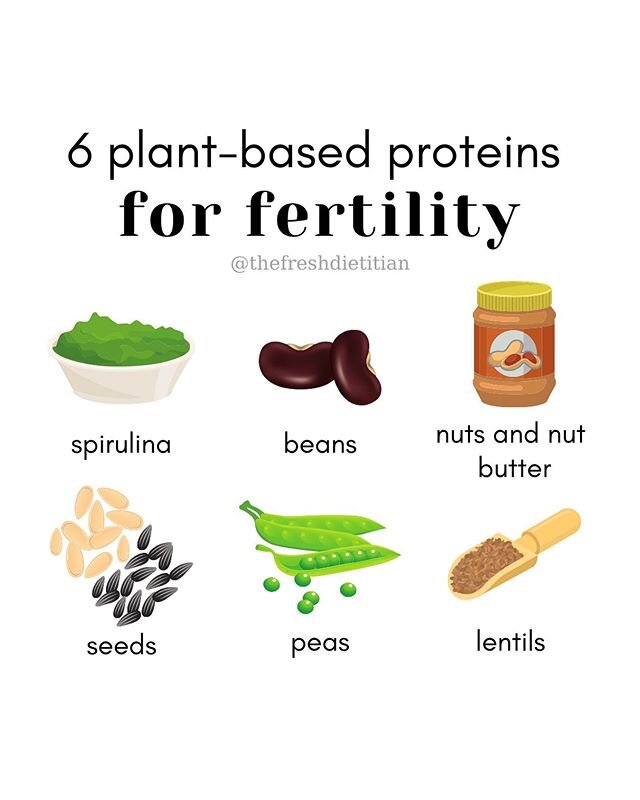
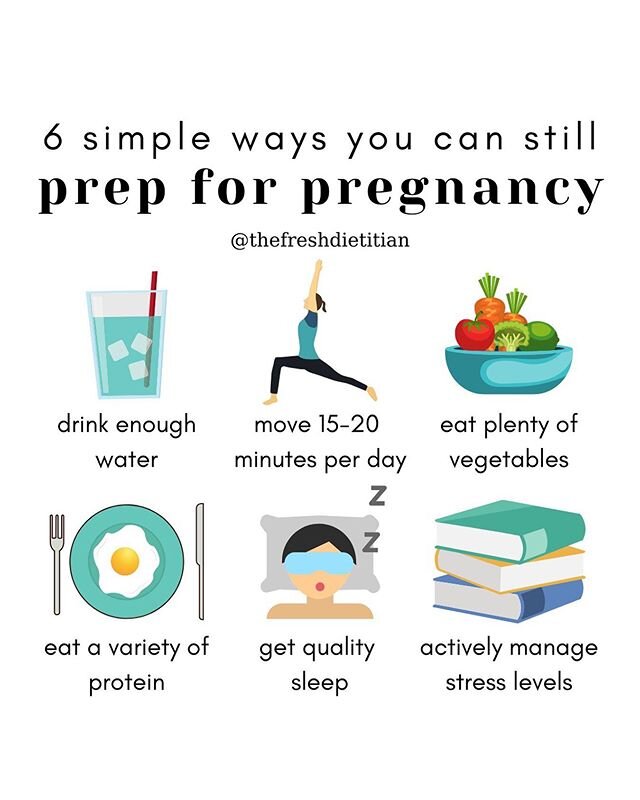
Eat a variety of proteins (poultry, beef, dairy, plant-based, and seafood)
Protein is literally the building block of our bodies and we need to be consuming enough to not only support our cycle but support the demands of pregnancy. Getting in the habit of eating adequate amounts of protein from a variety of sources can help carry that habit throughout pregnancy where protein needs increase dramatically.
Consume seafood at least 2x per week
Seafood is not only a great source of protein but contains many other important nutrients such as the omega-3 fatty acids DHA and EPA, iodine, iron, and zinc (to name a few). All of these nutrients help support the functioning of your thyroid and the growth and development of a fetus.
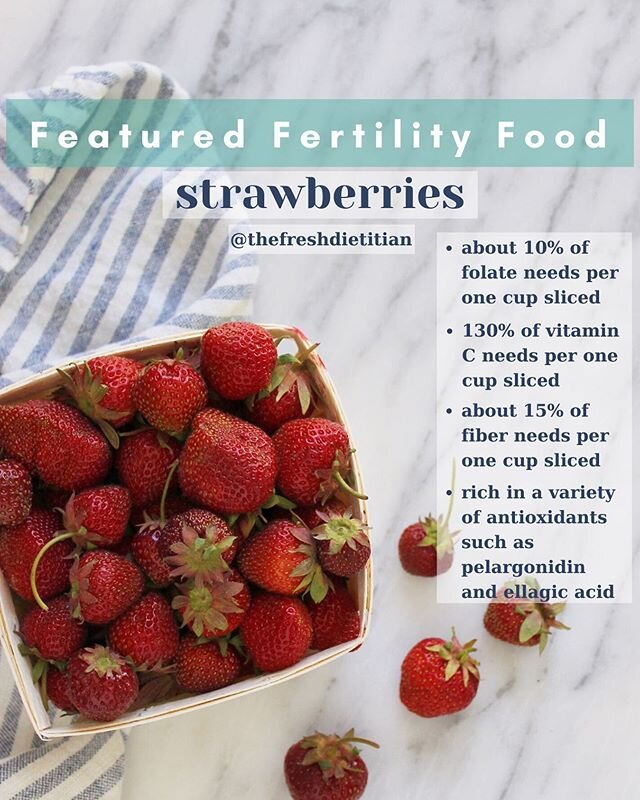
Eat the rainbow daily (lots of colorful fruits and vegetables)
Eating the rainbow invites variety, which helps fuel a healthy and diverse gut microbiome. Your gut is vital in many things but when it comes to your cycle, you gut helps you properly metabolize hormones. (When the hormones are done with sending their message, they need to be metabolized and excreted.) Eating the rainbow also ensures you consuming a variety of antioxidants – important for minimizing oxidative damage, protecting and improving egg quality, and promoting healthy brain and neural development in a growing baby.
Get vitamin D checked
We are uncovering more and more about vitamin D’s role in fertility and pregnancy. Unfortunately, it’s also one of the most common nutrient deficiencies around. Sunlight is the best source of activating vitamin D but that entirely depends on where you live, what season it is, the weather that day, sunscreen use, etc. It’s always good to get vitamin D checked to see where your levels are and make appropriate changes to make sure you’re sufficient.
Visit your dentist/hygienist
There is a direct connection between oral health and fertility (in both male and females). Make it a habit to regularly visit your dentist, have your teeth cleaned, and get ahead of any potential issues such as developing gum disease.
Improve sleep quality
Sleep is vital to cycle health and maintaining a healthy HPA/HPO axis. You want to aim for a minimum of 7 hours of sleep, going to bed at a consistent hour, and going to bed well before 11 AM to maximize your body’s chances of entering long stretches of deep sleep (the most rejuvenating phase of sleep).
Implement active stress management
Stress is not something we just simply “have to deal with”. In fact, elevated, consistent levels of cortisol (your stress hormone) can interrupt your brain’s ability to communicate with your ovaries causing cycle interruptions and potentially cause anovulatory cycles (or cycles where you don’t ovulate). If there’s no egg released to fertilize, pregnancy can’t happen. Implement a routine that brings you back down to Earth. Incorporate hobbies that you love, spend time in nature, move your body in a way you enjoy, read a book, take a bubble bath - whatever it is that helps you feel calm and restored.
Don’t be afraid to ask for help or seek additional information
The “rule” that you need to wait 1 year of having unprotected sex (or 6 months if you’re over the age of 35) before reaching out for help with your fertility is bullshit. If you suspect something is wrong and you want to investigate, you have the right to do so. You’re not being overly cautious or dramatic. You’re being proactive. I’ve had plenty of clients who came to me with seemingly normal cycles but when we got to digging, we uncovered things that needed significant improvement before the body was ready to support a pregnancy. (Read about recommended tests here.) Don’t be on anyone else’s timeline except your own. You have a right to seek help when YOU want to.
If you’re looking for ways to optimize your fertility or answers to improve your chances of getting pregnancy, I’m accepting one-on-one clients and would love to be your guide. Apply to work with me here.
What labs are recommended if you’re having hormone or fertility issues?
If you’re struggling issues such as:
- irregular periods
- heavy, painful periods
- fertility issues
- severe PMS symptoms (mood swings, irritability, tender breasts, cramping)
- fatigue or sleep issues
- low libido
…it’s likely due to hormonal issues. Hormones are used as a means of communicating throughout the body to give the body direction or tell it to do something. Insulin, for example, helps the body regulate glucose levels by letting glucose into cells. Hormones are messengers or signals and when there are hormonal issues, it’s usually a sign that your body is trying to tell you something.
Best thing to do is to test, not guess.
There are a number of lab tests you can do to collect data about your cycle and fertility health. These are the most popular ones I order and analyze for my clients.
DUTCH Complete or DUTCH Cycle Mapping
DUTCH tests are one of my favorites because they provide a deep dive into overall cycle health by measuring a variety or hormones and hormone metabolites (compounds after the body has processed the hormones). DUTCH tests are not invasive and do not require a blood draw as everything is measured via urine collection.
The DUTCH test(s) measure(s):
- estrogen (sex hormone)
- progesterone metabolites (sex hormone)
- DHEA (androgen hormone)
- testosterone (sex hormone)
- androstenedione (androgen hormone)
- cortisol (stress hormone)
- melatonin (sleep hormone)
- organic acids (measure a variety of things such as: neurotransmitter metabolites, oxidative stress, and nutrient levels)
The two most frequent DUTCH tests I order are called DUTCH Complete or DUTCH Cycle Mapping and Complete bundle. Both tests include everything listed above but the DUTCH Cycle Mapping has you collect over the course of your entire cycle so it allows you to see the where in your cycle you have estrogen peaks and how much progesterone was released and how long it was sustained. This allows us to see 1) if you ovulated, 2) when in that cycle you ovulated, and 3) the quality of that ovulation.
Everything is connected within the body – hormone systems, reproductive systems, digestive systems, etc. DUTCH results can clue us in to other things that need attention. Certain patterns of hormone levels can tell us whether the thyroid may be playing role or whether the gut needs to be looked into further.
Full thyroid panel + antibodies
Thyroid plays a major role in fertility and pregnancy so if you have symptoms such as brain fog, fatigue, sensitivity to cold or temperature changes, heavy periods, frequent and large clots during your period, or fertility issues, it’s a good idea to get a full thyroid panel.
As opposed to simply measuring TSH (thyroid-stimulating hormone), a full thyroid panel includes TSH, free and total T4, free and total T3, reverse T3, and thyroid antibodies (anti-TPO and anti-TG). A full thyroid panel gives you a complete picture of thyroid function and can clue you in to whether your thyroid is contributing to your fertility issues.
Vitamin D
Vitamin D plays a crucial role in fertility and pregnancy and is a very common nutrient deficiency. Having your vitamin D checked provides you a baseline that you can then work from. If you’re deficient, you’ll want to work with a healthcare professional to increase your levels and be re-checked after 3 months to see how they’ve improved.
Fasting insulin and glucose
Your ovaries are responsive to insulin. When there’s too much insulin present in the blood (hyperinsulinemia), it can contribute to interruptions in ovulation. Having insulin and glucose measured together allows you to determine if you’re insulin resistant. Having insulin resistance can increase your risk of developing Type II diabetes and gestational diabetes during pregnancy. Learning ways to manage insulin resistance prior to getting pregnant can help regulate cycles and help you go on to have a healthy pregnancy.
Hemoglobin A1c
Hemoglobin A1c is a 3-month average of your blood glucose levels. This value goes hand-in-hand with fasting insulin and glucose and can be used in the diagnosis of diabetes.
Anemia panel
Iron deficiency is the most common nutrient deficiency in our country. Iron is needed to transport oxygen in the blood and is crucial to the proper growth and development of a fetus. Checking your iron status can help identify an issue that can be remedied prior to getting pregnant and reduce the risk of complications developing. Anemia panels should include serum iron, ferritin, transferrin, total iron binding capacity, and sometimes folate and B12 levels.
Variety of fertility hormones (AMH, FSH, LH, estradiol, progesterone)
AMH or anti-Muellerian Hormone is a measurement of ovarian reserve. AMH should be measured along with other fertility hormones to provide an overall picture of fertility health. FSH and LH are hormones released to initiate ovulation. Estradiol is a major sex hormone also released to initiate ovulation (among many other roles). Progesterone is the hormone released after ovulation and can be used to determine if you ovulated and the quality of that ovulation.
Prolactin
Prolactin is the hormone released in the highest amounts during lactation/breastfeeding. However, certain conditions can increase levels (hyperprolactinemia) and can cause amenhorrea and ultimately lead to infertility. If your cycles are sporadic or infrequent or missing, getting prolactin levels measured is important to rule out as a cause.
hs-CRP
C-reactive protein (hs = high sensitivity) is a measure of inflammation. Research has shown that women with unexplained infertility and diminished ovarian reserve had higher levels of circulating CRP compared to women with normal ovarian reserve. Measuring CRP along with an anemia panel can help determine what role (if any) inflammation may be playing in iron status.
Gut microbiome
You’re probably wondering what your gut has to do with your fertility. But as I mentioned earlier in this post, your gut is connected to the way you metabolize and process hormones, which can contribute to cycle health or cycle interruptions. Doing an in-depth stool analysis can give you an overview of your microbiome (or a breakdown of the organisms that live in your gut such as parasites, fungi, beneficial bacteria, opportunistic bacteria, protozoa, as well as general digestive health). If you have digestive issues, this is one way to potentially determine a root cause and have a protocol developed to help relieve you of those problems.